Just as the monarch butterfly undergoes a profound transformation—struggling to emerge from its chrysalis with newfound wings—women also experience a significant life shift: menopause. This stage, often misunderstood or ignored, isn’t an ending but a metamorphosis filled with strength, wisdom, and resilience.
In the workplace, women navigating menopause bring immense value—experience, leadership, perspective, and emotional intelligence. But like the unspoken rule of Fight Club, menopause is often a topic we don’t talk about. That silence comes at a cost.
It's time to break the stigma. Workplaces must recognize menopause as a natural, powerful transition and offer the support women need to thrive. Because keeping women in the workplace—valued, supported, and empowered—isn’t just the right thing to do; it’s essential for a thriving, balanced, and innovative workforce.
With 26% of women globally over 50 —and living longer —this aging workforce offers institutional knowledge and stability companies can’t afford to lose. The SWAN study highlights that post-menopausal women report better mood and focus, free from hormonal fluctuations. Menopause is a workforce imperative. Each year, 1.3 million U.S. women transition into menopause, with 6,000 reaching it daily. Researchers link the unaddressed needed workplace support to a $26.6 billion annual economic loss from absenteeism and healthcare costs. Why pay attention? Menopause impacts productivity and retention. The U.S. Bureau of Labor Statistics shows women aged 55-64 have a 64.1% employment rate, dropping to 18.9% past 65—indicating many exit prematurely. HR must bridge this gap to retain talent through the transition. Let’s begin with the story of the monarch butterfly; then we will share how this metaphor relates to menopause.
In the heart of nature, where life's most profound changes unfold, lies the tale of the monarch butterfly.
Its journey, a radical metamorphosis, begins with a tiny egg, soon hatching into a larva, the monarch caterpillar. For days, it nourishes itself, growing and shedding its skin, preparing for the next stage of its remarkable development.
Then comes the chrysalis, a seemingly quiet phase. But within this jade casing, an extraordinary process begins. The caterpillar, in essence, liquefies, breaking down completely. Imagine: a complete internal restructuring. The old form dissolves, making way for the new. Specialized cells, dormant until now, begin to build the magnificent adult butterfly from this biological essence. It's a powerful act of letting go to allow for something stronger to emerge.
And then, the emergence. The butterfly, transformed, breaks free. It rests, gathers its strength, and with newfound wings, takes flight – more capable, more vibrant than before.
This incredible process mirrors another significant transformation in life: menopause. Like the chrysalis, it can feel like a period of profound and sometimes uncomfortable change. There can be discomfort, a feeling of things shifting and changing in ways that are unfamiliar. It can feel messy, like the liquefaction within the chrysalis. But this breakdown is essential for the powerful rebuilding that follows.
Menopause, typically occurring between ages 45 and 55, is a significant transition for women, marking the end of reproductive years. While often associated with challenges like hot flashes, mood changes, and cognitive shifts, menopause also brings unique strengths that can enhance workplace contributions. With 80% of women experiencing menopause while working, recognizing and supporting these benefits is critical for fostering an inclusive, productive work environment.
The largest growing segment of the workforce is women over 45 . And yet, when they experience symptoms that impact their work, many are met with dismissal, discomfort, or outright discrimination. 70% of women surveyed over the age of 55 stated they felt invisible and only 32% men felt invisible as they aged in a study by Gransnet.
Just as the monarch emerges stronger and ready for its journey, women in their post-menopausal years often find themselves with renewed energy, clarity, and purpose. Many describe it as one of the most productive and rewarding phases of their lives.
We understand the vital role of the monarch in our ecosystem. We recognize its journey, its resilience. In the same way, we must recognize and value the incredible experience and strength that women bring to our workforce and our communities, especially after this powerful transformation.
Menopause is a natural biological transition, yet it remains under-addressed in healthcare systems and workplace environments. Menopause is the natural time in a woman’s life when her periods (menstrual cycles) stop permanently because the ovaries no longer release eggs or make as much of the hormones estrogen and progesterone. It is officially diagnosed after 12 months without a menstrual period (not caused by pregnancy, illness, or other reasons).
Perimenopause is the transitional phase leading up to menopause, during which a woman’s body begins to undergo hormonal changes as it moves toward the end of reproductive years.
More specifically:
It is marked by fluctuating levels of estrogen and progesterone, the main female sex hormones.
It typically begins several years before menopause (often in a woman’s 40s, but can start earlier).
Perimenopause ends one year after the final menstrual period, which is when menopause is officially reached.
Common signs and symptoms include:
Irregular menstrual cycles (shorter, longer, heavier, or lighter than usual)
Hot flashes and night sweats
Sleep disturbances
Mood changes or irritability
Vaginal dryness
Decreased fertility
There is no test for menopause. Hormone tests, such as those measuring estrogen or FSH, are not a reliable way to diagnose menopause because these hormone levels change constantly—sometimes even hour by hour. A blood test only shows the hormone level at that one moment, not what’s really happening in the body over time. For this reason, experts like NICE (the UK’s National Institute for Health and Care Excellence) and the British Menopause Society recommend diagnosing menopause based on a woman’s age and symptoms—such as hot flashes, sleep problems, or changes in periods—rather than blood tests. Hormone testing is only useful for younger women, usually under 40, when doctors suspect early menopause or another condition affecting the ovaries.
Recent studies highlight the significant personal and economic costs of untreated menopausal symptoms, underscoring the urgent need for systemic change. To understand a woman today going through menopause and the confusion she experiences with treatment options, we will begin with some history.
The New York Times article titled “Women Have Been Misled About Menopause” outlines how women have been poorly educated and misinformed about menopause, leading to unnecessary suffering and stigma. Here’s a succinct summary of the key findings:
In the late 1990s, ~15 million women annually were prescribed hormone replacement therapy (HRT).
After the Women's Health Initiative (WHI) study linked HRT use to an increased risk of cardiovascular events and breast cancer, there was:
A drop in prescriptions of HRT by 70% by 2009, due to misinterpretation of small risk increases.
An immediate noticeable employment decline among women aged 40–55 years — suggesting that untreated menopause symptoms may have pushed many women out of the workforce.
The breast cancer risk increase reported was 26%, but in real terms, this meant a rise from 2.33% to 2.94% over 10 years—a marginal absolute risk.
For every 10,000 women on hormones, about 8 more would develop breast cancer compared to those not taking them.
Positive Impact of HRT:
Further analysis found that among women aged 58–70, use of HRT was associated with a 32.6% increase in short-term employment.This suggests that managing menopause symptoms effectively (e.g., through appropriate HRT use) can improve women's ability to remain in the workforce, supporting both individual economic security and broader economic productivity.
Medical Education Gap
A 2017 survey found:
20% of medical residents received no menopause lectures.
⅓ said they would not prescribe HRT, even to low-risk symptomatic women.
Half of U.S. gynecologists are under 50 and were trained after the WHI study, when menopause education was largely abandoned.
Many women in the above study were in their 60’s and 70’s.
Today, new research is providing a more nuanced understanding of how HRT affects not just the body, but also the brain.
A 2025 study from the UK Biobank explored how different patterns of HRT use relate to women’s brain health, using advanced brain imaging and prescription data. The findings offer an updated perspective: while HRT does not appear to cause major harm or offer broad brain protection, its effects can vary depending on factors such as age at use, duration, and surgical history.
Menopausal hormone therapy and the female brain
Researchers studied over 20,000 women in the UK to see how hormone replacement therapy (HRT) affects the brain during and after menopause.
They compared women who:
currently use HRT,
used it in the past, and
never used it.
Brain scans and prescription data were used to measure brain aging and memory-related brain areas.
What they found
Current HRT users had brains that looked slightly older (about 9 months older) and had smaller hippocampal volumes (a brain region important for memory).
Longer use and older age at last use were linked to more signs of brain aging.
Women who had a hysterectomy or ovary removal and took HRT had younger-looking brains than those who hadn’t had surgery.
No clear difference was found based on type of hormone, dosage, or method (pill vs patch).
Having a gene linked to Alzheimer’s (APOE ε4) didn’t change the results.
What this means
The study suggests:
HRT does not strongly protect the brain,
but also does not cause major harm.
Its effects depend on individual factors like age, duration, and surgical history.
Bottom line
HRT can help with menopause symptoms like hot flashes, but its impact on brain health is mixed. Women should discuss personal risks and benefits with their doctor to decide what’s best for them.
This widespread gap in menopause education has left both clinicians and patients navigating a landscape of uncertainty and outdated information. Without consistent, evidence-based training, many providers lack the confidence to guide women through this important stage of life—often relying on incomplete or misunderstood data from decades past. Unfortunately, this confusion is further compounded by ongoing and sometimes conflicting research.
For example, a recent headline from July 2, 2025, reignited public concern:
“Study finds link between certain types of hormone therapy and higher rates of breast cancer.”
In this study, researchers reported an association between specific forms of postmenopausal hormone therapy and increased breast cancer rates before age 55, prompting renewed debate and anxiety among women already seeking clarity on safe treatment options.
A new study of women having hormone therapy after menopause found a link between a certain type of treatment and higher rates of breast cancer before the age of 55. CBS News medical contributor Dr. Celine Gounder joins "CBS Mornings" to explain.
November 2025 the FDA black box warning was taken off HRT hormone replacement therapy; a term when used at my local Costco, was unfamiliar to the pharmacy tech. She understood a brand name or generic medication name but not HRT. Shouldn’t pharmacists understand the term hormone replacement like they understand antibiotics without saying give me a brand name I don’t know what you are referring to?
This confusion and neglect underscore a deeper systemic problem: menopause is a medical condition with identifiable symptoms and recognized presentations, yet it continues to be treated as secondary or less serious than other health concerns.
Tragically, this failure to prioritise menopause care has had devastating consequences. As The Guardian reported, a coroner recently raised serious concerns about how the NHS supports women during menopause following the death of a 54-year-old teacher who took her own life after a severe decline in her mental health.
“Menopause is a condition; it does have symptoms and it does have recognised presentations, yet there appears to be a failure to recognise this condition as having equal importance to other ailments or diagnoses.” A Coroner has expressed wide-ranging concerns about how the NHS cares for women during menopause after the death of a 54-year-old teacher who killed herself after a decline in her mental health. The Guardian
This heartbreaking case is not an isolated tragedy—it reflects a broader failure to recognize menopause as a critical health issue deserving of serious medical attention and compassionate care. It is heartbreaking to learn within my lifetime as a woman, the medical profession has identified women in perimenopause and menopause as ‘whiny women, whiny gynies, madame Dolores, tbd-total body dolor, status Hispanic,’ per Dr. Mary Claire Haver.
Despite its profound impact on women’s physical and mental well-being, menopause remains under prioritized and misunderstood within healthcare systems worldwide.
Recognising this gap, leading researchers and clinicians have called for a new approach. According to “Menopause: Time for a Paradigm Shift,” published in Mayo Clinic Proceedings (2023), the data paint a stark picture:
Vasomotor Symptoms (Hot Flashes and Night Sweats)
Approximately 75% of women undergoing menopause experience vasomotor symptoms (VMS), such as hot flashes and night sweats, which can persist for over 7 years on average. These symptoms are far from merely uncomfortable—they often disrupt sleep, increase risk for anxiety and depression, and erode overall quality of life. Importantly, the burden of VMS is not experienced equally across all groups. Black and Latina women report more frequent and severe VMS than their white counterparts. In fact, data from the Study of Women’s Health Across the Nation (SWAN) show that Black women have both a higher prevalence and a longer duration of hot flashes—often extending beyond 10 years.
The Menopause Rating Scale (MRS), which assesses physical, psychological, and urogenital symptoms, averaged 12.1 among study participants, reflecting a moderate symptom burden. However, symptom severity varies significantly across groups. Latina women, for instance, are more likely to report heightened psychological symptoms, such as depression, anxiety, and mood instability. Black women, meanwhile, are more likely to report genitourinary symptoms, including bladder issues and vaginal dryness.
Healthcare Gaps and Intersectional Challenges:
Despite the widespread and long-lasting impact of menopause, many women—particularly those from marginalized communities—struggle to access adequate care. Socioeconomic barriers, and cultural stigma contribute to health disparities. Finding clinicians who are both menopause-trained and culturally competent in gender-diverse care is often difficult, exacerbating delays in diagnosis, lack of treatment, and social isolation.
…women with symptomatic menopausal transition may have a higher risk of development of subsequent psychiatric disorders, especially depressive disorder, anxiety disorder, sleep disorder, and bipolar disorder.~Risk of Psychiatric Disorders Following Symptomatic Menopausal Transition
While the physical and emotional toll of vasomotor and psychological symptoms is undeniable, it’s equally important to recognize what’s happening within the brain during this transition. Menopause is not only a hormonal and systemic shift—it is also a profound neurological recalibration.
The Enlightened Brain: How Menopause Restructures and Adapts
What’s remarkable about all this new research is that it reframes menopause not as a story of loss, but as one of reorganization and renewal. Neuroscientists like Lisa Mosconi and Roberta Britton have helped us see that the menopausal brain isn’t shutting down—it’s restructuring.
During perimenopause, as estrogen levels fluctuate and drop, the brain experiences a temporary dip in gray-matter volume and glucose metabolism—essentially, it’s recalibrating. But with time, it adapts to its new hormonal environment. Neural networks reorganize. Metabolism stabilizes. Energy pathways shift from glucose toward fatty acid utilization, and new receptor patterns emerge. The 2021 Scientific Reports study demonstrated that by post-menopause, the brain’s energy production actually improves, showing resilience and metabolic flexibility.
This is the neurological parallel of enlightenment: a shedding and rebuilding process. Just as emotional and spiritual growth often follows a period of uncertainty or dismantling, the menopausal brain undergoes its own metamorphosis. It is not breaking—it’s becoming.
Mosconi’s more recent PET imaging studies (2024) even show increased estrogen receptor density across the transition, suggesting that the brain is actively tuning itself to function optimally in a changed internal landscape. Brinton’s work on neuroimmune and metabolic remodeling reinforces this view: menopause initiates a creative restructuring, a process that demands energy, adaptation, and—ultimately—wisdom.
Seen through this lens, menopause becomes not just a biological turning point, but a neurological awakening. The brain’s restructuring mirrors the psychological and spiritual adaptations many women describe—a deepened clarity, renewed focus, and a shift in priorities that comes not despite hormonal change, but through it.
As we begin to see menopause through this lens of adaptation and neurobiological renewal, it challenges old narratives—not just in medicine, but in how we design systems that claim to “understand” women. The science shows that the female brain is dynamic, resilient, and capable of profound restructuring in response to hormonal change.
Which raises a timely question for our modern era: What will we teach AI about women?
As AI becomes increasingly integrated into healthcare — sometimes even taking the lead — it holds immense potential to revolutionize how we understand and support women through every stage of life, including menopause. Yet the promise of these technologies depends on how they are built and whose experiences they reflect.
Will AI be good for women’s health? Only if it learns from the right data. Medical research has always treated men as the default — excluding women from trials until 1993, when the NIH finally required their inclusion. Entire generations of health datasets were built on male bodies, leaving dangerous gaps in how we understand women’s health, from heart attack diagnoses to menopause care. Today, these gaps persist and risk being amplified by biased algorithms. If we want AI to truly serve women’s health, we must teach it the full story — one that honors women’s experiences not as data outliers but as essential truths.
What will AI engineers feed into the systems shaping our future? Will they include the realities, strengths, and needs of women in menopause?
AI mirrors the humans who train it; our values become its vision. So let’s ensure that vision includes every woman. Advocate for better data, inclusive design, and workplace innovation that recognizes menopause as a stage of power and potential — not decline. Together, we can teach AI, and the world, to see women in their fullest strength and ensure the future generations are advocated for.
If we want AI to truly serve women’s health, we must teach it the full story — one that honors women’s experiences not as data outliers but as essential truths. Menopause is a profound transformation that deserves attention not only in clinical care but in research and technology design.
Across academia, researchers are beginning to address these very gaps. At Cornell University, for example, scientists have launched the Menopause Health Engineering initiative — a groundbreaking effort uniting experts in biomedical engineering, medicine, and computation to unravel the science of menopause. Led by Dr. Nozomi Nishimura and Dr. Claudia Fischbach-Teschl, the team is confronting decades of bias in biomedical research that historically excluded women and overlooked the physiological complexity of menopause. Their work recognizes that conditions often labeled “aging diseases” — from cardiovascular disease to osteoporosis and dementia — manifest differently in women, demanding sex-specific models of research and care.
This initiative exemplifies a new academic movement: harnessing technology, interdisciplinary science, and inclusive data to close the gender health gap. Cornell’s researchers are developing advanced imaging systems, body-on-a-chip platforms, and computational tools to decode the biological and systemic changes of menopause. They are also embedding women’s health challenges into student research and clinical training, ensuring the next generation of engineers and physicians sees menopause not as an afterthought but as a vital part of human health.
Such work reflects the broader mission of teaching both AI and science to see women fully — to build systems, datasets, and therapies that reflect the realities of every stage of life.
Cornell’s Menopause Health Engineering initiative exemplifies the type of systemic recalibration needed to close enduring gaps in women’s health research. By uniting engineers, clinicians, and data scientists, the program recognizes that menopause is not a niche topic but a critical intersection of biology, technology, and policy. Its interdisciplinary framework — spanning advanced imaging, computational modeling, and multi-organ systems research — represents a shift toward understanding menopause as a central determinant of lifelong health, not an isolated event. This is how academia begins to rewrite the biomedical narrative: by generating inclusive data, training future researchers to ask sex-specific questions, and embedding women’s experiences at the core of health innovation.
It is within this evolving landscape that the meaning of menopause itself is being redefined. Menopause is not an ending, but a profound transformation — a chrysalis moment leading to a powerful new flight. It calls for sustained inquiry, systemic advocacy, and the courage to reimagine both science and society through an inclusive lens. As emerging research demonstrates, the post-menopausal years are not a period of decline but one of potential — a phase in which many women experience their greatest productivity, leadership, and contribution. Understanding and supporting that transformation through evidence-based research and technological innovation is not just good science — it is essential to achieving equity in health and opportunity.
Embrace the change, trust the process, and witness the beauty of emerging stronger. Many women find that post-menopausal years are among the most productive and rewarding of their careers.
Menopause can amplify emotional intelligence, a key leadership asset. Research suggests women navigating menopause develop heightened self-awareness and emotional clarity, translating into stronger interpersonal skills like empathy and conflict resolution. A 2019 study by Jack, Riach, and Bariola found that post-menopausal women often exhibit greater agency, leveraging life experience.
Post-menopausal women excel at understanding diverse perspectives, making them adept at managing teams and fostering collaboration. Empathy, as noted in neuroscience research, activates the brain’s reward system, enhancing workplace connection. With years of experience, these women often make decisive, clear choices, providing strong direction. Workplaces that promote women into leadership roles during this phase can harness their ability to build trust and inspire teams.
Despite stereotypes of menopause as disruptive, many women report improved focus post-transition. A 2011 study by Greendale, Derby, and Maki notes that cognitive challenges during perimenopause often stabilize post-menopause, leading to enhanced concentration.
Studies show that women with access to menopause-specific workplace resources, like flexible hours or wellness programs, report higher productivity and better mental health. Life experience enables women to prioritize effectively, tackling complex projects efficiently. Navigating menopause fosters resilience, equipping women to handle workplace stress with composure. Employers can leverage this by assigning high-impact projects to women in this stage, trusting their precision and focus.
Menopause often empowers women to advocate for themselves and others including embracing mentorship roles, sharing knowledge and championing inclusivity. Their lived experience makes them attuned to diverse needs, advocating for policies like menopause-specific benefits—which 64% of women desire but only 14% feel employers recognize.
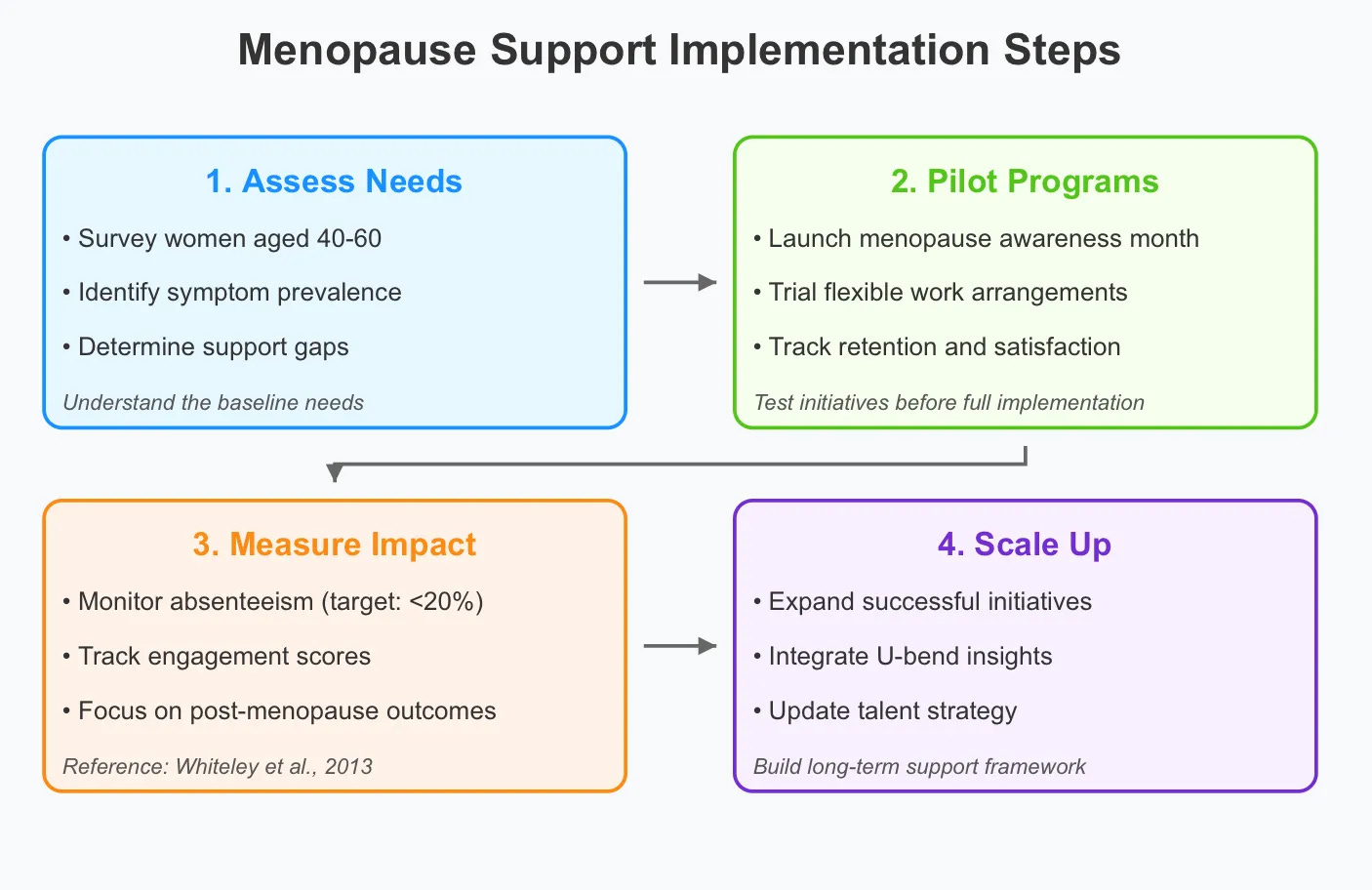
To harness these benefits, employers must create supportive environments. Menopause -friendly policies are gaining traction in some countries, but global adoption lags. Practical steps include:
Flexible Work Arrangements: Remote work or adjustable hours help women manage symptoms like fatigue or hot flashes, which 72% of women report feeling self-conscious about at work, and leave policies that recognize the often debilitating effects menopause causes.
Education and Awareness: Training managers reduces stigma, normalizing menopause. Launch workshops to demystify menopause—only 55% of women understand it pre-transition.
Health Benefits: Access to menopause-specific healthcare, covering hormone therapy, and mental health resources to support women’s whole well-being.
Comfortable Workspaces: Temperature controls or fans alleviate physical discomfort, boosting focus.
Companies offering menopause-specific benefits include those in the tech sector like Adobe and Nvidia, as well as firms in other fields like Bank of America and Bristol Myers Squibb, and Genentech. TIME—Now’s The Time to Bring Up Menopause At Work
Bank of America—Break Through the Stigma Menopause in the Workplace Study and Findings
NVIDIA—Menopause Support with PEPPY
Supporting menopausal women is a strategic advantage.
The U-bend of happiness suggests women’s life satisfaction often dips in midlife but rises after age 50; however, longitudinal studies like the Edmonton Transitions Study show happiness increasing from young adulthood to midlife without a consistent dip (Galambos et al., 2015). Post-menopause, women over 55 in a Russian longitudinal study reported increased life satisfaction, potentially due to more personal time and community engagement (Kolosnitsyna et al., 2017). The U-shape is not universal, as cultural, socioeconomic, and gender differences create diverse happiness trajectories, challenging a singular midlife low for women (Laaksonen, 2018; Steptoe et al., 2015).
According to the Fawcett Society’s 2021 report, menopause-friendly workplaces see lower turnover and higher satisfaction. With one billion women globally navigating menopause, the ripple effect of support is profound—reducing loneliness, as harmful as smoking 15 cigarettes daily, and enhancing morale.
By valuing the emotional intelligence, focus, and advocacy of menopausal women, organizations tap into a talent pool driving innovation. Menopause isn’t just a challenge—it’s an opportunity to redefine women’s contributions at work.
Menopause-Related Workplace Support and Legal Developments
As companies seek innovative ways to attract and retain top talent, menopause-related support is emerging as a new frontier in employee well-being and inclusion.
Legal and Policy Landscape
Rhode Island became the first U.S. state (effective June 2025) to explicitly protect employees experiencing menopause or related conditions under its Fair Employment Practices Act. Employers must provide reasonable accommodations—such as flexibility for managing symptoms—and notify employees of these rights.
Rhode Island FEPA — § 28-5-7.4 (Accommodation of Pregnancy-related and Menopause-related Conditions) Text of amended Fair Employment Practices Act (FEPA), now including menopause.
Key provisions in statute:
It is unlawful for employers to refuse reasonable accommodation for an employee’s or prospective employee’s condition related to pregnancy, childbirth, menopause, or related medical conditions.
Employers cannot require leave if other accommodation is possible.
Employers must provide written notice of rights (posted and provided to employees).
Definitions include “reasonable accommodation” and what constitutes related conditions (e.g., managing vasomotor symptoms).
The bill’s enacted text comes from 2025-S 0361/H 6161, which amended the original language to explicitly add menopause protections.
Other states are following suit. Illinois and Louisiana require insurance coverage for menopause treatments, while New York has introduced multiple bills expanding workplace awareness and protection.
Illinois House Bill 5295 / Public Act 103-0703 (2024) — Insurance Coverage for Menopause
Amends 215 ILCS 5/356z.56 so that group or individual health insurance must provide coverage for medically necessary hormonal and non-hormonal therapy to treat menopausal symptoms (effective Jan 1, 2026).
Adds corresponding coverage requirements for Medicaid under 305 ILCS.
New York Senate Bill S7495 (2025-2026) — Enacts the Menopause Awareness Improvement Act: establishes a menopause education program and directs study of impacts on the workforce.
https://legislation.nysenate.gov/pdf/bills/2025/A8542
https://legislation.nysenate.gov/pdf/bills/2025/S7495
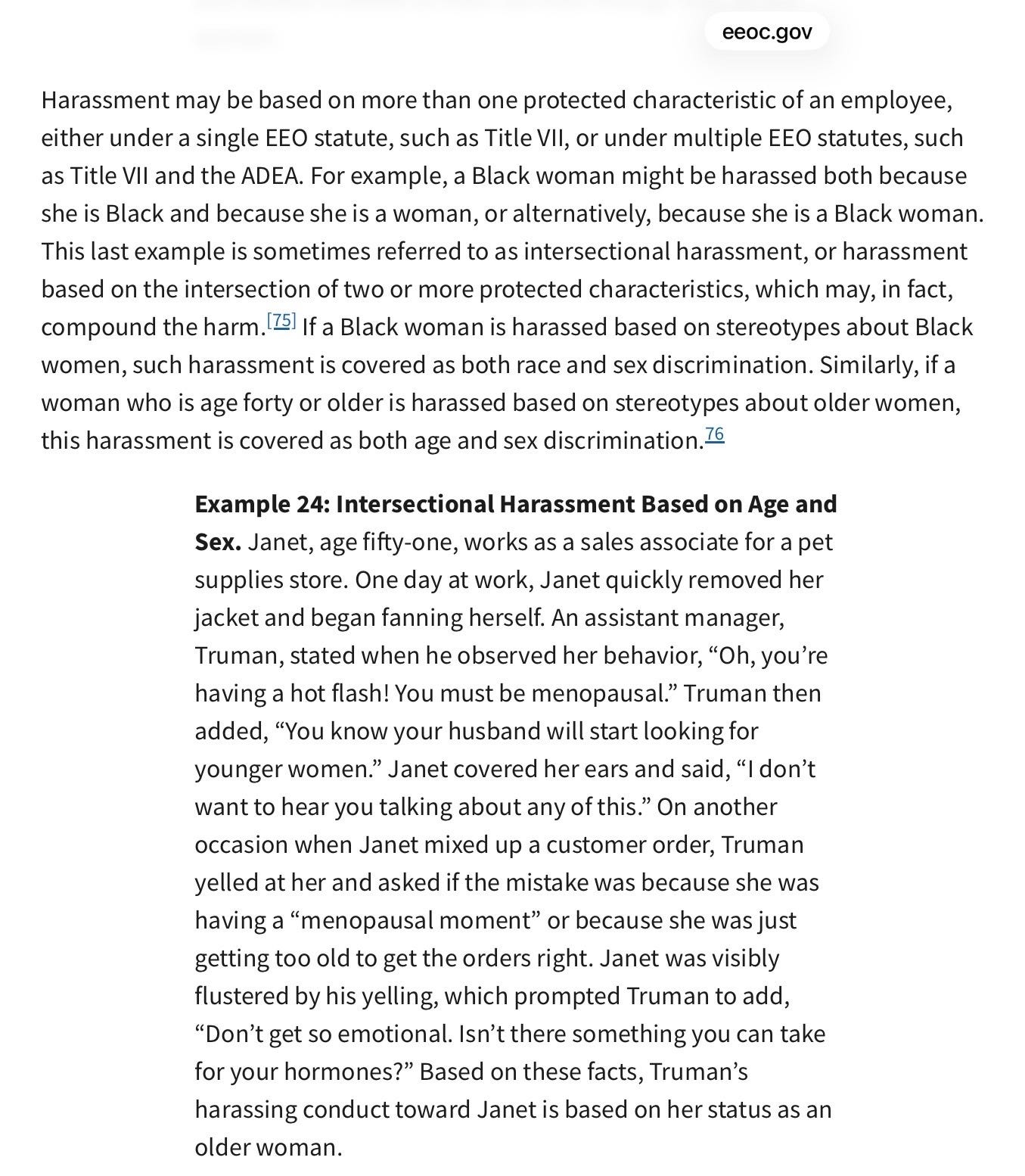
Federal laws such as the ADA, FMLA, and Pregnant Workers Fairness Act (PWFA) may also cover certain menopause-related conditions, though interpretations are still evolving. The EEOC’s 2024 guidance warns that menopause-related teasing or stereotypes can constitute harassment based on sex and age. (page 24).
TIME Magazine article, Newsom Dropped the Ball on Menopause, But Other States Are Ready to Lead, “California Governor Gavin Newsom vetoed the Menopause Care Equity Act, a bill, AB 432: The Menopause Care Equity Act, that had passed the state legislature with near-unanimous bipartisan support.”
California Assembly Bill 432 (2025-2026) — Menopause / Menopause Care Equity Act Requires mandatory menopause-related continuing medical education for physicians with ≥25 % women patients.
Requires health insurers and health care service plans to cover evaluation and treatment options for perimenopause and menopause (when issued, amended, or renewed on/after Jan 1, 2026). https://trackbill.com/bill/california-assembly-bill-432-menopause/2649698/?utm
Workplace Implications
Despite its prevalence, menopause support has historically been fragmented under general disability, leave, or antidiscrimination laws. However, growing legislative attention to reproductive health (e.g., pregnancy and prenatal leave laws) signals a cultural and policy shift toward recognizing menopause as a legitimate workplace issue. There also are no current safety guidelines for women at work.
OSHA—Occupational Safety and Health Administration
The General Duty Clause is found in Section 5(a)(1) of the Occupational Safety and Health Act. It requires employers to provide a workplace free from recognized hazards that are causing or are likely to cause death or serious physical harm. In simple terms: if a hazard is known, foreseeable, and preventable, employers have a duty to address it—even when there’s no specific OSHA standard spelling it out.
1. OSHA’s General Duty Clause
Under the General Duty Clause, employers must provide a workplace “free from recognized hazards that are causing or are likely to cause death or serious physical harm.”
Menopause-related symptoms can become workplace hazards when conditions aggravate them, such as:
Excessive heat
Poor ventilation
High stress
Lack of access to restrooms or drinking water
Rigid uniforms or PPE
If employers know these conditions are affecting workers and do nothing, it may raise OSHA concerns.
2. Heat Stress and Temperature Control
Hot flashes and thermoregulation issues make menopausal workers more vulnerable to heat stress, which OSHA already recognizes as a hazard.
Relevant OSHA considerations:
Indoor heat exposure
Outdoor work in high temperatures
Lack of cooling, fans, or climate control
Heavy PPE that traps heat
Menopause can increase risk, making existing heat hazards more serious.
3. Ergonomics and Fatigue
Symptoms like joint pain, muscle stiffness, sleep disruption, and fatigue can increase the risk of:
Slips, trips, and falls
Repetitive strain injuries
Reduced concentration leading to accidents
OSHA views fatigue and ergonomic strain as safety risks, even if the underlying cause is medical.
4. Sanitation and Access Requirements
OSHA requires:
Adequate restroom access
Potable drinking water
Clean facilities
These are especially important for menopausal workers who may need:
More frequent restroom use
Hydration to manage symptoms
Privacy for symptom management
Restricting access can become an OSHA compliance issue.
5. PPE and Uniforms
OSHA requires PPE to be:
Properly fitted
Appropriate for the worker and task
Menopause symptoms may make standard PPE unsafe or intolerable (e.g., heavy, non-breathable clothing), increasing heat stress or discomfort that affects safety.
6. Stress and Psychosocial Hazards
While OSHA has limited enforcement in this area, it recognizes that:
Excessive stress
Long shifts
High workloads
can contribute to safety incidents. Menopause can amplify stress-related risks, making accommodations a preventive safety measure.
7. Increasing Recognition (Though Not Yet Regulated)
OSHA has not issued menopause-specific rules, but:
Menopause is increasingly discussed in workplace safety and health guidance
Some employers include menopause in safety risk assessments and wellness programs
It intersects with ADA, Title VII, and workers’ compensation considerations
OSHA doesn’t regulate bodies. It regulates hazards. Heat, fatigue, poor ventilation, inflexible PPE, lack of restroom access, long shifts—those are already recognized workplace hazards. Menopause doesn’t create new hazards; it makes workers more vulnerable to the ones you already acknowledge and manage every day.
If heat stress is a safety issue, it doesn’t stop being a safety issue because the worker experiencing it is a 52-year-old woman instead of a 25-year-old man. If fatigue increases injury risk, it doesn’t suddenly become “personal” when sleep disruption is hormone-related. The hazard didn’t change—your workforce did.
This isn’t about feelings, politics, or special treatment. It’s about applying the General Duty Clause consistently to a workforce that includes people who don’t look like the men who wrote the original safety manuals.
Ignoring menopause doesn’t make workplaces safer. It just means you’re dismissing a known, foreseeable risk—exactly what the General Duty Clause was designed to prevent.
Bottom Line
Menopause is an OSHA issue when:
Workplace conditions worsen menopausal symptoms
Those symptoms increase safety risks
Employers fail to address known, preventable hazards
It’s not about menopause itself being regulated—but about workplace hazards interacting with a common biological life stage that affects a large portion of the workforce.
Until guidance from OSHA is given, employers can…
Extending menopause benefits voluntarily can demonstrate leadership in inclusion and talent strategy but may raise compliance or fairness issues if not carefully structured.
Employers should review existing leave and accommodation policies, monitor legislative changes, and train managers on respectful, compliant responses to menopause-related needs.
Rhode Island’s law represents a turning point in recognizing menopause as both a workforce and equity issue. As awareness spreads, forward-thinking employers that integrate menopause-inclusive policies will strengthen employee well-being, retention, and diversity—positioning themselves at the forefront of modern workplace support.
Resources for your workforce
The role of lifestyle medicine in menopausal health: a review of non-pharmacologic interventions—IMS White Paper—Lifestyle choices are powerful medicine. Through nutrition, movement, rest, stress reduction, and social connection, women can take charge of menopause with strength, balance, and vitality—reducing reliance on medications and promoting lifelong health.
Women’s Bureau US Department of Labor guide for your leadership: LET’S TALK ABOUT IT: MENSTRUATION AND MENOPAUSE AT WORK
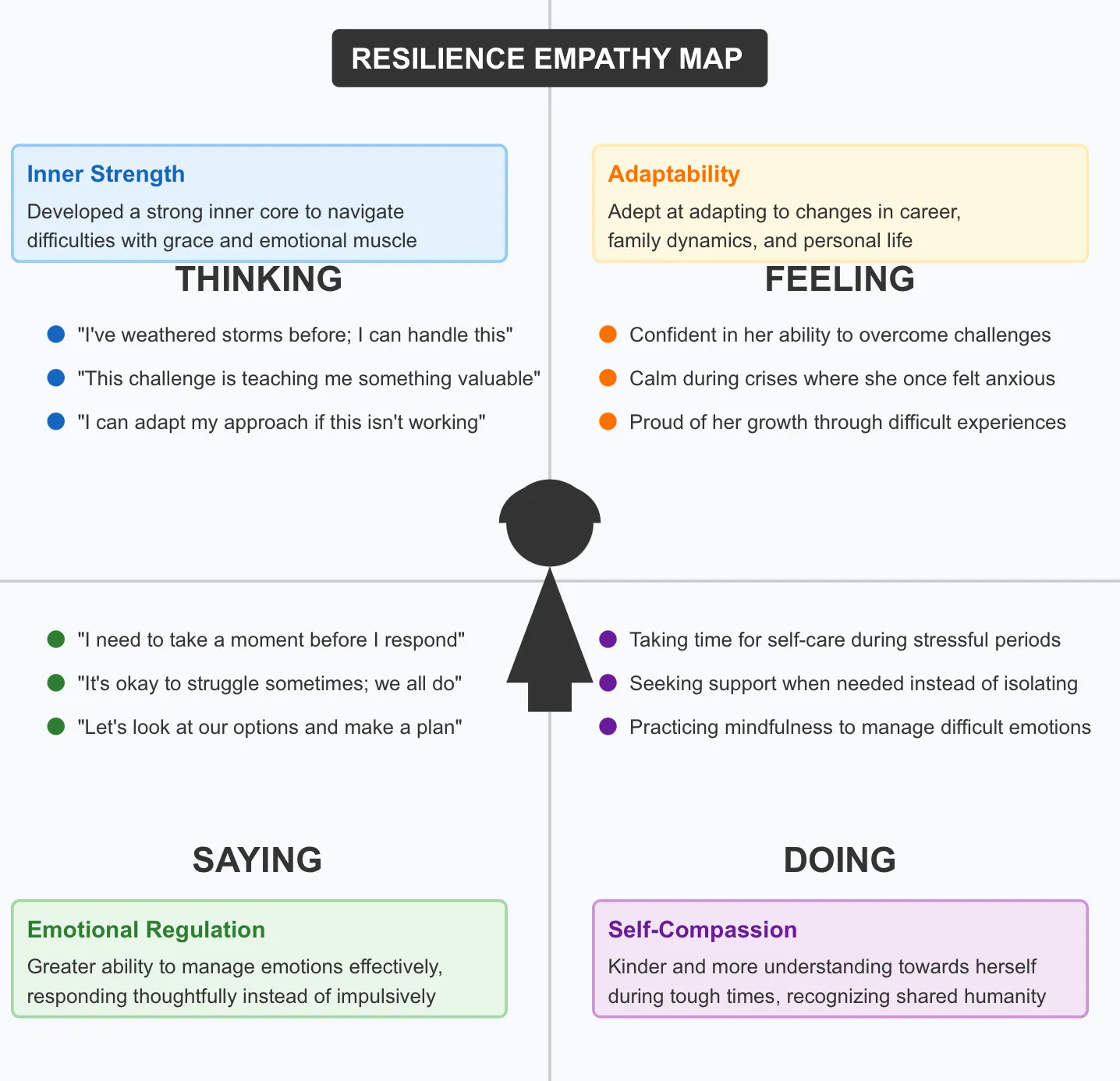
Peer led communities at work tool— Have conversations on a weekly basis to foster hope. Bring women who have experienced the transition to support the younger women. Focus on the benefits with the following empathy map. Present each topic area, and ask questions related to what each woman is thinking, feeling, saying and doing. Set goals in each area with small steps to take daily. Let each person choose one area to work on between meetings reporting back on progress. Celebrate small accomplishments. This will foster a growth mindset with hope.
Connect with our LinkedIn Group—Redefining Happiness in Menopause
📢Menopause Belongs in Workplace Conversations
Contact your lawmakers today and urge them to support legislation protecting workers experiencing menopause—because fairness, dignity, and health belong at work.
Every worker deserves dignity, fairness, and understanding—at every stage of life. Menopause affects more than half of the workforce, yet outdated policies leave many without the accommodations or protections they need. Rhode Island has led the way by explicitly protecting employees experiencing menopause under its Fair Employment Practices Act, and other states are beginning to follow. It’s time for lawmakers nationwide to act. Join us in calling for legislation that ensures workplaces provide reasonable accommodations, prevent harassment or discrimination, and recognize menopause as a key component of gender equity and worker well-being.
It’s time to protect workers’ rights through every stage of life. Rhode Island has set the standard—now it’s your state’s turn. Use this letter template to advocate for change.
Subject: Support Legislation Protecting Workers Experiencing Menopause and Related Conditions
Dear [Senator/Representative/Governor _____],
I am writing as a concerned constituent to urge you to support and champion legislation that explicitly protects employees experiencing menopause and related health conditions in the workplace.
In June 2025, Rhode Island became the first state in the nation to recognize menopause as a protected condition under its Fair Employment Practices Act, requiring employers to provide reasonable accommodations—such as flexible scheduling or access to cooling or rest areas—and to inform employees of these rights. This historic step acknowledges a reality faced by millions of workers and ensures they are treated with dignity, fairness, and equity.
Other states are taking action as well. Illinois and Louisiana have mandated insurance coverage for menopause treatments, while New York has introduced bills expanding workplace awareness and protections. These developments reflect a growing recognition that menopause, a natural life transition, can meaningfully impact health, productivity, and career advancement—and that our policies must evolve to meet these needs.
At the federal level, the Americans with Disabilities Act (ADA), Family and Medical Leave Act (FMLA), and Pregnant Workers Fairness Act (PWFA) may offer partial coverage, but these protections are inconsistent and dependent on interpretation. The Equal Employment Opportunity Commission (EEOC)’s 2024 guidance further warns that menopause-related teasing or stereotypes can constitute harassment based on sex and age—highlighting the urgent need for clear, enforceable laws at every level. (page 24).
By passing legislation to protect workers experiencing menopause and related conditions, we can:
Promote fair and inclusive workplaces for all genders and life stages;
Reduce stigma and discrimination related to natural biological processes;
Support retention of experienced workers and strengthen our workforce; and
Set a national standard for equitable treatment in employment and health care.
I respectfully ask that you support—or introduce—legislation modeled after Rhode Island’s policy to ensure that no worker faces bias or job insecurity due to menopause-related symptoms. This is a commonsense, bipartisan opportunity to advance workplace equality and public health.
Thank you for your leadership and your commitment to protecting the rights and well-being of all workers.
Sincerely,
[Your Full Name]
[Your Address]
[City, State, ZIP]
[Email / Phone Number]
WORLD MENOPAUSE DAY 10/18/25 LINKED IN LIVE VIDEO ON YOUTUBE—psychosocial education for men and women—Alexia Georghiou
We posted a CNN article in the sub Reddit r/menopause, People worldwide don’t know enough about menopause. Here’s why that’s dangerous, 12.4.25…may the comments give voice to women’s experiences shared in the thread. May they be heard.
📢 Join our confidential menopause focus group to share your experiences and help shape better support for women’s health and wellbeing. Your voice matters—fill out the Menopause Focus Group Interest Form
Menopause Matters: Supporting Women in the Workplace
BY ALEXIA GEORGHIOU, FOUNDER, KNOXVILLE HAPPINESS COALITION
Published in HR Pulse by the American Society for Healthcare Human Resources Administration December 2025